What is atrial fibrillation?
What is AF? AF (or Afib) is a common type of irregular heart rhythm. AF is a medical abbreviation which means ‘atrial fibrillation’. This term refers to the atria (the two upper chambers of the heart which receive blood from your veins and push this blood into your ventricles). It also refers to fibrillation, meaning to quiver or contract spontaneously.
AF occurs when the atria experience chaotic electrical signals, causing them to ‘quiver’ rather than contract in a coordinated manner. This irregular and rapid electrical activity can disrupt the normal heart rhythm and lead to a variety of symptoms and potential health issues.

What are the symptoms of atrial fibrillation?
AF is associated with a range of symptoms, but not everyone with AF presents noticeable symptoms. Some people may have ‘silent’ AF, where the condition is detected during routine medical checkups – in other words, they do not experience the overt symptoms of atrial fibrillation. Other people may display typical symptoms simultaneously, such as heart palpitations and tiredness.
When symptoms of atrial fibrillation are present, they can vary in severity. The following are the most common symptoms of Afib:
1. Palpitations
The most common symptom of atrial fibrillation is heart palpitations. Atrial ‘flutter’ symptoms are a fluttering sensation or irregular, or rapid, beating of the heart. A heartbeat of more than 100 beats per minute is considered rapid – you can check your own heart rate by feeling your neck or wrist and counting the beats per minute.
Heart palpitations can last for a few seconds up until a few minutes. Some people describe this as a ‘quivering’ of the heart. Others may describe the sensation as twitching, fluttering, or spasming in the chest.
2. Fatigue
An AF heart condition can cause persistent tiredness or a lack of energy. This is due to the heart’s inefficient pumping of blood, which hinders the oxygen and nutrient rich blood which is distributed around the body. This can cause tiredness, sluggishness and fatigue.
3. Shortness of Breath
Some individuals with AF may feel breathless, especially during physical activity or exertion. This is because the heart works harder to meet the body’s demand for oxygen. An elevated heart rate can lead to an increased respiratory rate, making you feel like you’re out of breath.
4. Chest Pain or Discomfort
Chest pain, pressure, or discomfort may occur in people with AF, although it is less common than in other heart conditions like angina. If someone is experiencing anxiety or stress due to atrial fibrillation, this may manifest as chest discomfort or a feeling of tightness.
5. Dizziness or Lightheadedness
Afib can lead to a drop in blood pressure and reduced blood flow to the brain, resulting in dizziness or a feeling of lightheadedness. The severity of dizziness in AF can vary from person to person.



When should I be worried about an irregular heartbeat?
Everyone experiences a fluttering sensation in their hearts at some point during their lives; this ‘skipping a beat’ feeling can be brought on by a number of emotions, including excitement or nervousness.
However, you should go and see your doctor if you are experiencing frequent, rapid palpitations that last for a prolonged period of time. Remember, a rapid heartbeat is more than 100 beats per minute, and you can measure this at home by feeling your wrist or neck. You should also schedule an appointment if you experience chest pain or breathlessness. Your doctor can run some tests to see whether these palpitations are harmless or a sign of an underlying condition.
How is atrial fibrillation diagnosed?
If your doctor suspects you have atrial fibrillation, they will conduct a few tests to determine this. First, a pulse test is carried out, where your heartbeats will be measured within a time frame. A pulse of more than 100 beats per minute is an indication of atrial fibrillation.

The next step in diagnosis is an electrocardiogram (ECG), which measures the electrical activity of the heart and can detect an irregular pulse.
Finally, blood tests may be conducted to check for underlying conditions that could be causing or contributing to AF, such as thyroid problems or electrolyte imbalances.
Atrial fibrillation treatments
Treatment for atrial fibrillation depends on a person’s age, overall health, type of AF and underlying causes. The first step of treatment will be to determine any underlying causes for an AF heart condition. For example, if you have an overactive thyroid gland (hyperthyroidism), treating it may also cure atrial fibrillation.
If no underlying causes of atrial fibrillation can be found, treatment options can include the following:
1. Rate Control
The primary goal of rate control is to slow down the excessively fast and irregular heart rate associated with atrial fibrillation. A normal resting heart rate of fewer than 90 beats per minute can be achieved using drugs for atrial fibrillation. These include beta-blockers or calcium channel blockers.
2. Rhythm Control

Rhythm control aims to restore and maintain a normal heart rhythm. This can be achieved through various methods. The first is an electrical cardioversion, which delivers an electric shock to the heart to reset its rhythm to normal.
Catheter ablation can also control an irregular pulse. Ablation is a procedure which involves using catheters (thin tubes) to create scar tissue in the heart. This can help break up the electrical signals that cause rapid, irregular heartbeats.
Finally, antiarrhythmic medications are drugs which help maintain a normal heart rhythm and prevent AF recurrences.
3. Anticoagulation (Blood-Thinning) Therapy
Atrial fibrillation is associated with an increased risk factor for heart attack or stroke, due to the risk of blood clots in the atria. Typical drugs for atrial fibrillation are blood thinners, which may be prescribed to reduce the risk of stroke by preventing blood clot formation. The choice of blood thinner depends on individual risk factors and preferences.
4. Lifestyle Changes
Living with atrial fibrillation requires some lifestyle changes to help manage the condition. These include managing underlying health conditions, such as high blood pressure and diabetes; achieving and maintaining a healthy weight; and regular physical activity (which is possible and actively encouraged, bearing in mind some precautions).

5. Implantable Devices

Some individuals with an AF heart condition may benefit from implantable devices like pacemakers or implantable cardioverter-defibrillators (ICDs) to help control heart rhythm or manage complications.
My heartbeats are not constantly irregular – what does this mean?
If your irregular, rapid heartbeat seems to ‘come and go’, you may have what is known as paroxysmal atrial fibrillation (medically abbreviated as ‘paf’). In paf, abnormal heart rhythms occur intermittently and spontaneously but then return to normal rhythm on their own, usually within a few days. These episodes can last for a few seconds, minutes, hours, or even days, but usually cease on their own.
Paroxysmal atrial fibrillation can occur as a result of the same triggers as atrial fibrillation; namely poor diet, smoking, caffeine, alcohol and stress. As we have mentioned before, both forms of atrial fibrillation can also be caused by underlying health conditions, such as thyroid problems, that should be identified before starting any treatment.
What does af mean for my lifestyle?
When you first get diagnosed with Afib, it is important to take time to understand your condition and not to rush into any drastic life changes immediately. Make sure to read any resources given to you by your doctor, and go to your appointment with questions you have thought about in advance.
Once you have understood exactly what atrial fibrillation is, your doctor will speak to you about treatment options. However, outside of medical intervention through treatment, there are lifestyle changes that you should consider making that will help reduce your symptoms and the health implications of the condition.
Make sure to consult your doctor before making the following lifestyle changes:
1. Move towards a heart healthy diet

A heart-healthy diet can help control weight and blood pressure, which are important for managing AFib. Consider a diet rich in fruits, vegetables, whole grains, lean protein, and low in saturated fats, cholesterol, and sodium. Read our 15 Easy Food Swaps article for ideas.
2. Maintain a healthy weight
Being overweight or obese can increase the risk of atrial fibrillation and worsen its effects. Losing excess weight through a combination of diet and exercise can help.
3. Limit alcohol and caffeine
Excessive alcohol and caffeine consumption can trigger atrial fibrillation episodes in some people. Reducing or eliminating these substances from your diet may be beneficial.
4. Quit Smoking
Smoking is a significant risk factor for heart disease and can trigger and exacerbate AFib. Quitting smoking is one of the most important steps you can take for heart health.

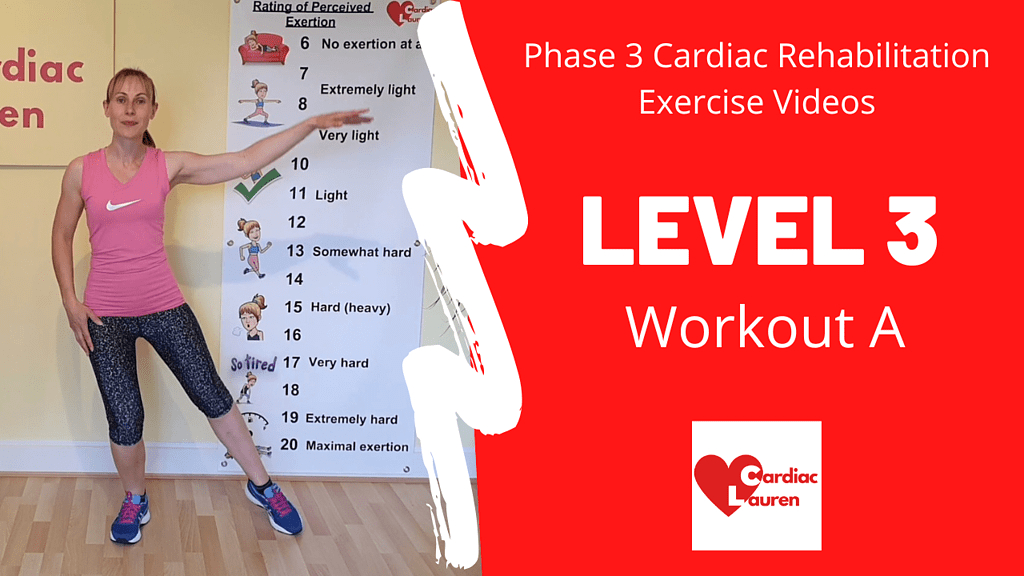
5. Exercise
Regular physical activity can help improve overall cardiovascular health. Cardiac Lauren is the perfect programme for people suffering from AF. Lauren will explain the importance of a 15-minute warm-up and 10-minute cool-down to help prevent further irregular heart rates and participants find they are able to cope with a full exercise session when they incorporate these elements. Please note that if you are using smartwatches and heart rate monitors to monitor yourself during an exercise session, be aware that they are not great at picking up your heart rate. They often ‘guess’ the rate as the atria are contracting at different times. Watch this short video explaining more HERE.
6. Manage Stress
High stress levels can trigger atrial fibrillation or make it worse. Practices such as relaxation techniques, yoga, meditation, or deep breathing exercises can help manage stress.

7. Stay Hydrated
Dehydration can trigger AFib episodes, so it’s essential to stay well-hydrated, but avoid excessive fluid intake.
Living with atrial fibrillation also means attending regular appointments with your healthcare practitioner, to check in, discuss symptoms and ensure that you are on the most effective treatment plan. It may also involve taking daily medications as directed by your doctor.

How long can you live with an irregular heartbeat?
AFib itself does not necessarily reduce life expectancy on its own. However, AFib is often associated with an increased risk of certain complications, such as stroke, heart failure, and other cardiovascular problems. If AFib is well-managed and a person receives appropriate treatment and makes lifestyle changes to control risk factors, their life expectancy may not be significantly affected.
Again, it is important to note that following the treatment and recommendations from your doctor is extremely important; this will ensure a minimal impact on your life expectancy. Although atrial fibrillation has been linked to a reduced life expectancy due to risks of stroke and heart failure, many people with atrial fibrillation also live normal lives.